Infertility is an increasing problem for all populations. The problem of fertility applies equally to the male and female sides. What are the most common causes of infertility? What do the steps for in vitro procedure look like? You will find the answers to these questions in our article.
Infertility is an increasing problem for all populations.The causes of infertility can be regionally differentiated and the percentage of individual causes will be different in Europe and for example in India – where this problem also exists, although it would seem to us that it is not there. In fact, the problem of fertility applies equally to the male and female sides. What else is worth knowing about infertility and IVF?
What are the most common causes of infertility?
Women often have menstrual disorders and irregular cycles, we postpone motherhood “for later” and as a result the potential for pregnancy decreases. The deeper the diagnosis, the more causes of infertility we can recognize. Men, in turn, have a tendency to decrease the quality of sperm all around the world.
Do you know how many couples trying to conceive may be affected?
It is estimated that about 20% of couples trying to conceive have a problem with becoming pregnant, i.e. every fifth couple. Unfortunately, these numbers are rising because women are delaying the implementation of reproductive plans, and age is a very important factor here, which unfortunately reduces the chances of getting pregnant. In addition, patients increasingly say that they do not have time to have sex. I will also mention that we are eating worse quality food, the percentage of obese people is increasing. The environment in which we live also has a significant impact on the functioning of the human body, including the quality of germ cells. The semen testing standards have been lowered several times over several dozen years due to its deteriorating quality even in donors of this semen. The problem of fertility problems simply won’t go away.
On what kind of help can a couple count on while being treated by Gyncentrum?
The first stage is diagnostics. A lot of information is already provided to us by the interview collected from patients. On this basis, we implement appropriate diagnostic procedures. When dealing with an infertile couple, we take into account the guidelines and recommendations of scientific societies, but it should be remembered that diagnostics, like the treatment itself, should be individual. It’s not always about doing as much research as possible, but about the right tests. Usually, at the initial diagnostic stage, patients are asked to perform hormonal tests, tests for the most common infectious diseases. Gentlemen, however, should do a sperm test. If necessary, patients are referred for further specialist consultations. Based on the patient’s history and ultrasound examination, many pathologies within the reproductive organ can already be suspected, which will require further diagnostic procedures, e.g. invasive diagnostics, such as laparoscopy or hysteroscopy. It should be remembered that diagnostics in infertility is still developing. Only after the diagnosis has been carried out, the treatment stage comes.
What is the most common treatment for a couple who wants to have a child before they are qualified for in vitro treatment?
In vitro is the most advanced procedure in infertility treatment and it is not necessary in all cases. Depending on the problem faced by the couple, the possible treatment will include the treatment for inflammation, complementary hormonal treatment and possible ovulation induction, intrauterine insemination with the semen of a partner or anonymous donor. If at the diagnostic stage it turns out that the fallopian tubes are obstructed, the method of choice becomes in vitro. There are many more indications for in vitro: more severe endometriosis, idiopathic infertility – when, despite numerous tests, no tangible cause of the lack of pregnancy or the so-called male infertility factor and many more.
What do the steps for in vitro procedure look like? When is the couple ready for this kind of treatment?
After performing a number of tests and other therapeutic methods, it may turn out that couple qualifies for in vitro fertilization. Sometimes patients find it difficult to come to terms with such a diagnosis. They need time and to talk together to somehow “get used to” the further plan for having children. If the decision is made, then yes, we proceed to the next steps. In vitro treatment involves stimulation for multiple ovulation, because the idea is to get more eggs than in the natural cycle, when usually only one egg is released from the ovarian follicle. To get more follicles with eggs, the patient undergoes hormonal stimulation, usually these are injections. Most patients tolerate stimulation time well, in some patients the ovarian response to given drugs is excessive and may develop so-called ovarian hyperstimulation syndrome. This is the most common complication of stimulation and luckily it is usually mild.
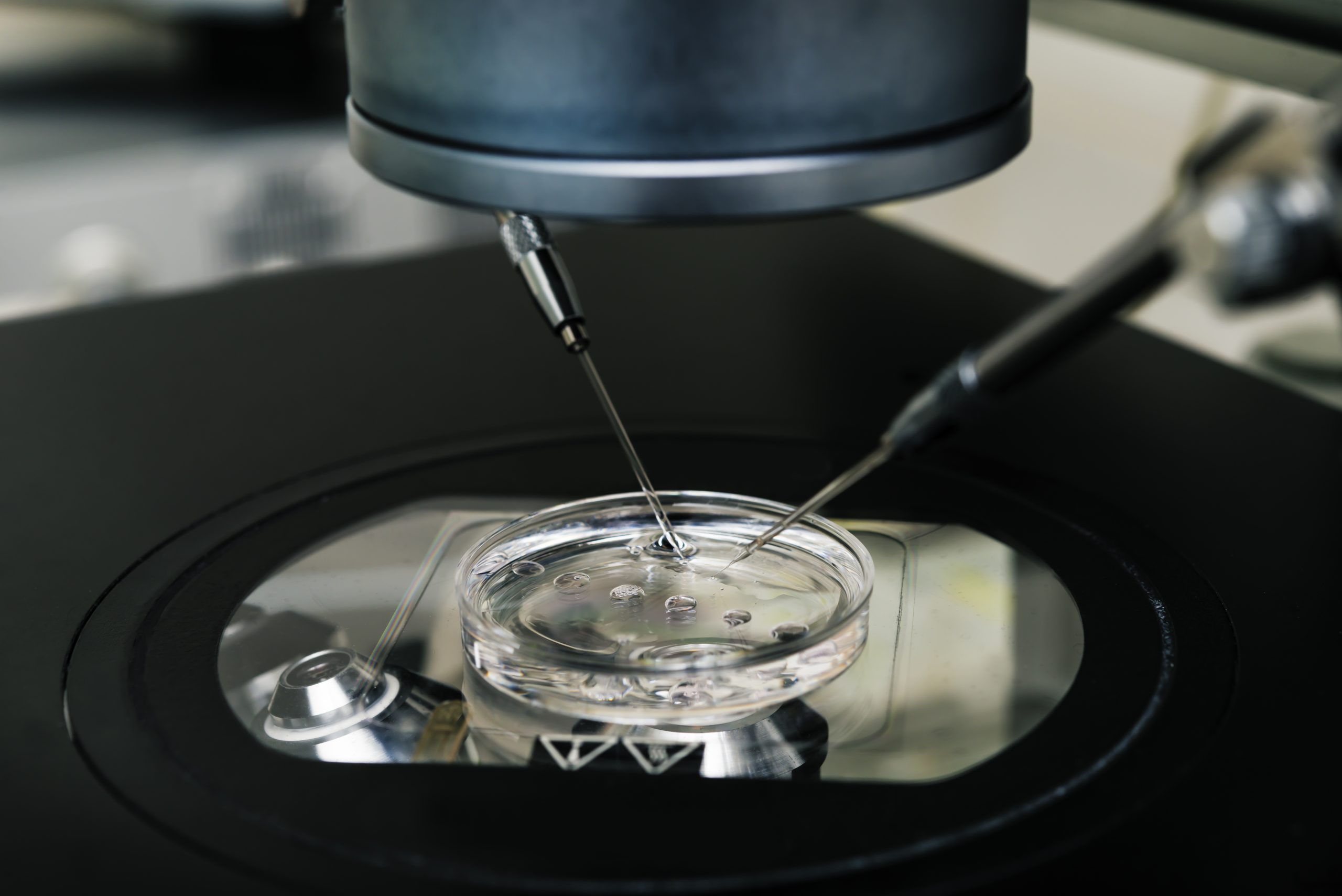
Stimulation ends with egg collection. The doctor decides when it occurs based on ultrasound monitoring and hormonal tests conducted during subsequent visits. Usually, it takes from 10 to 16 days from stimulation to the egg collection. It depends on the stimulation protocol that has been chosen for the patient, because sometimes all the hormonal preparation for puncture begins even several months earlier. Ovarian puncture involves taking egg cells from follicles. The procedure is performed with a special needle inserted into the vagina. All this happens under ultrasound control and is painless because the patient is anesthetized. After the procedure, abdominal discomfort and slight bleeding may appear. After the procedure, the patient remains for a short observation in the clinic, and in the meantime embryologists deal with follicular fluid collected from the ovaries. They look for eggs in it, clean them and evaluate their maturity. And now an important stage is coming – fertilization of eggs. If the fertilization was successful, embryologists observe how the embryos develop in the following days. Then, they check whether their pace of development is adequate and whether the morphology, i.e. the appearance of these embryos, is correct.
How does it look legally in Poland? How many eggs are collected, how many can you fertilize? What happens to the embryos?
The legal situation in Poland is regulated by the Act of 2015. According to it, 6 eggs can be fertilized, although during puncture the doctor collects fluid from all available ovarian follicles. Excess cells can be frozen. In some situations, such as the age of a patient over 35 or previous failed IVF procedures, or co-morbidities, the law allows the fertilization of more cells. The resulting embryos are cultured until the 3rd, 5th or 6th day. One embryo is transferred into the uterine cavity, sometimes two. Embryo transfer can be performed a few days after the egg collection or the resulting embryos are frozen and the transfer is deferred. The date of cryotransfer is decided by the doctor. The pregnancy test needs to be done from the blood to measure the level of chorionic gonadotropin-HCG 12 days after transfer (beta HCG test).
If couples have had unsuccessful in vitro tests, can you still diagnose at this stage why are you not pregnant?
Usually, patients who fail to succeed in vitro the first time, make further attempts. After the first unsuccessful procedure, we begin to search further for potential causes of pregnancy failure. We should remember that diagnostics in infertility is constantly developing, and the results of various scientific studies provide us with new information. Patients with reproductive failure may require further in-depth immunological, microbiological and genetic diagnostics. Sometimes, however, it turns out that the quality of the patients’ own germ cells, i.e. eggs and sperm, is very poor, and therefore embryos cannot be obtained. Then consider in vitro with donor oocytes or donor sperm.
When and in what cases do we carry out genetic tests? After miscarriages or can you do it sooner? Are embryos examined before transfer?
We often carry out genetic tests at the stage of diagnosis of infertility in both partners. Thanks to them, we can partially estimate the chances of pregnancy and the possible risk of embryo abnormalities. It is worth remembering that as parents age, the quality of their germ cells deteriorates and the risk of embryos occurring in chromosomal and genetic abnormalities increases significantly. Genetics are most often responsible for miscarriages of early pregnancies. There can be many reasons here, but thanks to research on aborted material we can learn a lot. In the case of in vitro use, it is possible to examine the embryo before it is given into the uterus. Thus, the chance that the given embryo will nest in the uterus increases and the pregnancy test result will not only be positive but a healthy baby will be born. We are talking here about embryo pre-implantation tests, such as PGT-A.
What is cryopreservation? Can you freeze eggs and sperm as well or just embryos? How many embryos can you freeze?
Cryopreservation consists in freezing cells and tissues. Currently, rapid freezing techniques are used with so-called vitrification method, which prevents the formation of small ice crystals that damage cells. You can freeze oocytes, semen and embryos themselves. According to Polish law, embryos created if their number exceeds the number of embryos to be transferred immediately after ovarian puncture (1 or maximum 2 embryos) must be frozen. Embryos must not be disposed of. If the couple no longer wants to have children, they should pay for the storage of embryos in the gamete and embryo bank or transfer them to the anonymous donation procedure to other couples in need.





